In the era of COVID-19, individuals concerned about their immune systems have an array of clinical options that may enhance their bodies’ ability to ward off pathogenic disease.
Although factors such as healthy lifestyle and optimal diet might seem more obvious in terms of building immune capacity, hormonal health actually plays a critical role in neutralizing viral infections such as those resulting from exposure to the novel coronavirus.
In this article, we’ll explore how testosterone levels affect the immunity as well as strategies to boost your own levels if you have a deficiency so that your immune system is prepared to defeat COVID-19 when you encounter it in your daily life.
Testosterone Levels Are Declining Alarmingly Quickly Among All Age Groups
Before we get into the science behind the interactions between testosterone and the immune system, it’s important to understand the testosterone deficiency epidemic that has gripped the US and the West at large.
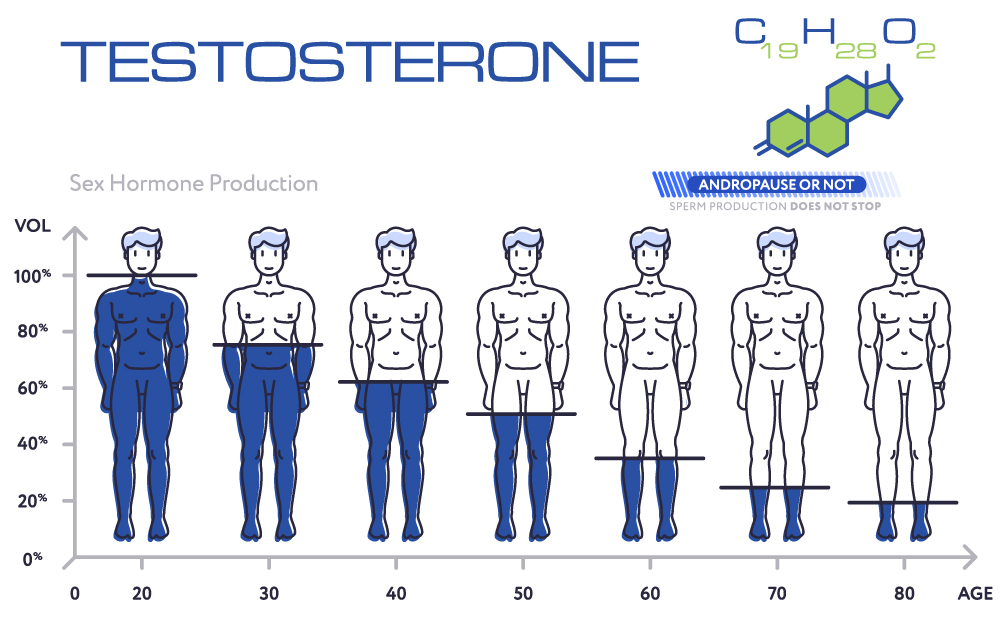
While testosterone deficiencies were once believed to only affect older men, a recent study on data collected by the National Health and Nutrition Examination Surveys (NHANES) found that, even among young men between 15-39 years of age, 20% were impacted by diagnosable testosterone deficiencies.
These hormonal deficiencies develop when the testes (the primary source of testosterone for men) fail to produce adequate amounts of the hormone – termed “hypogonadism” in the medical community.
What many may not realize is that testosterone plays a number of roles in health, not only for reproductive capability and sexual vitality.
Drops in testosterone levels have different causes depending on the individual, but they may include:
- Obesity (measured by body mass index).
- Lack of physical activity (sedentary lifestyle).
- Poor diet (especially ones high in processed foods and poor in zinc).
- Medications (including opioids and illegal steroids).
- Chronic inflammation.*
*Chronic inflammation is now widely understood to be a major driver of the most common diseases affecting Western populations, including heart disease, cancer, and metabolic disorders like diabetes. In addition, as we will discuss in detail below, inflammation is also closely linked to the cytokine immune response seen in severely ill COVID-19 patients.
A Balanced Immune Response Is the Key to Recovering From a COVID-19 Infection
While too much inflammation can be detrimental to health and even fatal, a balanced inflammatory response is a key component of the immune system’s activity – specifically, the innate immune response, the body’s frontline defense against unrecognized viral and bacterial invaders.
Inflammation initiates the activation of various immune system components to combat pathogenic infections, including:
- White blood cells (monocytes, neutrophils, lymphocytes).
- Antigens.
- C-Reactive proteins.
- Cytokines (critical for COVID-19 patients).
Cytokines regulate the activity of other types of cells involved in the innate immune response in a number of ways, including by modulating inflammation levels to either ramp up or tamp down immune system activity.
When cytokines fail to perform their work properly, they can trigger a potentially lethal “cytokine storm response.”
The Cytokine Storm Response and COVID-19
If you follow the news, you may be familiar with the so-called “cytokine storm response” in relation to COVID-19 fatalities.
While testosterone deficiencies were once believed to only affect older men, a recent study on data collected by the National Health and Nutrition Examination Surveys (NHANES) found that, even among young men between 15-39 years of age, 20% were impacted by diagnosable testosterone deficiencies.
These hormonal deficiencies develop when the testes (the primary source of testosterone for men) fail to produce adequate amounts of the hormone – termed “hypogonadism” in the medical community.
What many may not realize is that testosterone plays a number of roles in health, not only for reproductive capability and sexual vitality.
Drops in testosterone levels have different causes depending on the individual, but they may include:
- Obesity (measured by body mass index).
- Lack of physical activity (sedentary lifestyle).
- Poor diet (especially ones high in processed foods and poor in zinc).
- Medications (including opioids and illegal steroids).
- Chronic inflammation.*
*Chronic inflammation is now widely understood to be a major driver of the most common diseases affecting Western populations, including heart disease, cancer, and metabolic disorders like diabetes. In addition, as we will discuss in detail below, inflammation is also closely linked to the cytokine immune response seen in severely ill COVID-19 patients.
A Balanced Immune Response Is the Key to Recovering From a COVID-19 Infection
While too much inflammation can be detrimental to health and even fatal, a balanced inflammatory response is a key component of the immune system’s activity – specifically, the innate immune response, the body’s frontline defense against unrecognized viral and bacterial invaders.
Inflammation initiates the activation of various immune system components to combat pathogenic infections, including:
- White blood cells (monocytes, neutrophils, lymphocytes).
- Antigens.
- C-Reactive proteins.
- Cytokines (critical for COVID-19 patients).
Cytokines regulate the activity of other types of cells involved in the innate immune response in a number of ways, including by modulating inflammation levels to either ramp up or tamp down immune system activity.
When cytokines fail to perform their work properly, they can trigger a potentially lethal “cytokine storm response.”
The Cytokine Storm Response and COVID-19
If you follow the news, you may be familiar with the so-called “cytokine storm response” in relation to COVID-19 fatalities.
As we explored earlier, cytokines are an integral part of the immune response. They are necessary to trigger inflammation to neutralize a pathogen. However, in some cases (notably, for testosterone-deficient men) the cytokine response can “run amok,” triggering a deadly cascade of events that ultimately threatens the life of patients who experience these “storms.”
The central lessons to be learned are that controlling the inflammatory response of the immune system is critical to withstanding a COVID-19 infection and, more broadly, that maintaining a healthy immune system via hormonal regulation is an essential aspect of COVID-19 preparedness – particularly for individuals impacted by hormonal deficiencies.
How Testosterone Enhances Immune System Function
The clinical evidence is clear: testosterone exerts a direct influence over cytokine levels in the body. The findings in this study published in Aging Male offered two key takeaways critical to understand regarding testosterone and immune system function, specifically as it relates to the cytokine storm response:
- Men with testosterone deficiencies have higher levels of circulating cytokines.
- Testosterone replacement therapy (TRT) significantly decreases cytokine levels in men who have deficiencies.
Testosterone and Lung Health in COVID-19 Patients
The cytokine storm response, while it can impact the function of multiple organs, is primarily seen in hospitalized COVID-19 patients to impact the lungs.
This is the reason that many COVID-19 patients must be put on ventilators. Unfortunately, patients who must be assisted in breathing via ventilation experience much higher death rates than those who do not require ventilation.
Another study from the Elsevier Public Health Emergency Collection found that “low testosterone levels can cause a reduction of respiratory muscles activity and overall strength and exercise capacity, whilst normal circulating testosterone levels show a protective effect on several respiratory outcomes.”
The researchers go on to note that “a randomized controlled trial reported an improvement in peak oxygen consumption in men receiving testosterone replacement therapy.” Oxygen consumption levels are major predictors of COVID-19 survivability in patients who experience cytokine storm responses.
To support the findings of the Aging Male study cited above, the researchers also found, regarding the cytokine storm response, that “testosterone may have a role in the cascade of events leading to progression of COVID-19 infection due to the cytokine storm.”
They conclude that emergency medical providers should consider gauging the testosterone levels of incoming COVID-19 patients and, if the findings indicate a deficiency, to intervene to boost levels of the hormone as a prophylactic measure.
Testosterone Acts as an Immunomodulatory Agent
There is some understandable concern that, due to the tamping-down effects of testosterone on the cytokine response, that the hormone may inhibit the immune system’s capacity to combat pathogens such as COVID-19.
In fact, current research indicates that testosterone acts as an immunomodulatory agent (meaning it beneficially alters immune system function) rather than as an immunosuppressant.
The researchers in one study from the American Journal of Physical Anthropology found that “endogenous testosterone is associated with immuno-modulation, or at least selectively suppressive as opposed to broadly immunosuppressive.
Testosterone is associated with reduced cytokine responses following stimulation with a T-cell mitogen, PHA, while testosterone has no significant association with response to stimulation with a B-cell and monocyte mitogen, LPS.”
How to Safely Raise Testosterone Levels With Bioidentical Hormone Replacement Therapy (BHRT)
Given the breadth of evidence indicating optimal testosterone levels’ beneficial effects on the immune response, the question becomes how to safely elevate circulating levels of the hormone to enhance immunity.
Certainly, lifestyle factors such as more sleep, more physical activity, and a cleaner diet are shown to increase testosterone levels. These adjustments may correct minor deficiencies.
In some patients, though, clinical intervention is required to achieve the restoration of optimal testosterone levels in men with more severe deficiencies.
EvexiPEL performs all-natural testosterone replacement therapy using bioidentical hormone “pellets.”
“Bioidentical” refers to testosterone supplements that perfectly match the chemical composition of natural testosterone produced in the male testes and elsewhere in the body. The human body does not know the difference between endogenous testosterone and bioidentical testosterone introduced through therapy.
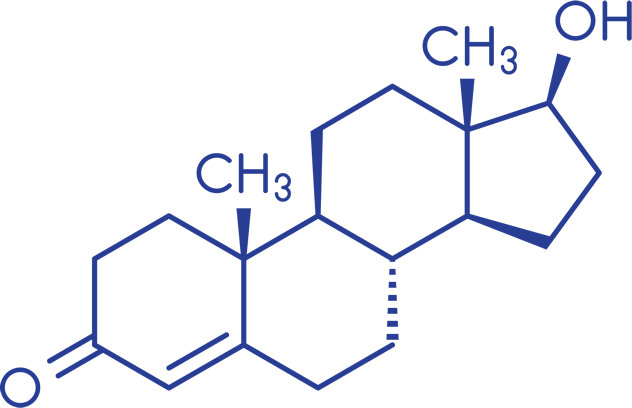
Testosterone
Bioidentical testosterone pellets are implanted under the skin with a small incision, releasing testosterone in incremental amounts over the course of weeks or months.
The providers at EvexiPEL monitor patients’ critical health markers before, during, and after therapy to ensure both the effectiveness and the safety of the therapies in patients who receive them.
Contact an EvexiPEL Certified Provider today to fortify your immune system and reap the many other substantial health benefits of optimized testosterone levels.
These hormonal deficiencies develop when the testes (the primary source of testosterone for men) fail to produce adequate amounts of the hormone – termed “hypogonadism” in the medical community.
What many may not realize is that testosterone plays a number of roles in health, not only for reproductive capability and sexual vitality.